Understanding Pulmonary Edema and Its ICD 10 Code
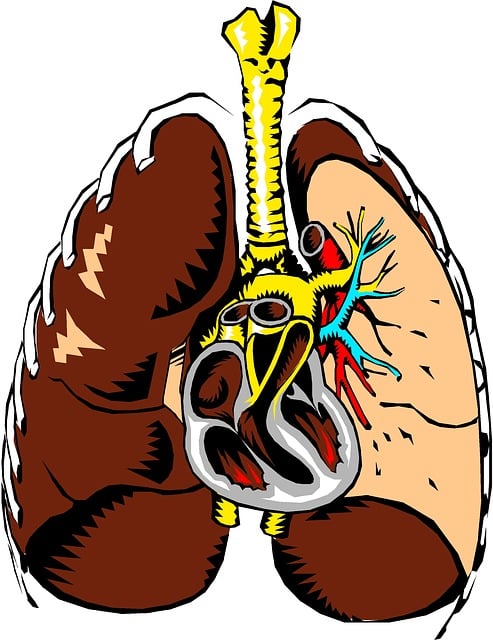
Pulmonary edema is a condition characterized by the accumulation of fluid in the lungs, leading to breathing difficulties and impaired oxygen exchange. The ICD 10 code for pulmonary edema is J81. This coding system is crucial for healthcare professionals to accurately document and track the prevalence of this condition. Understanding the ICD 10 code for pulmonary edema enables efficient communication and billing within the healthcare system.
Differentiating Pulmonary Edema from Pleural Effusion
It’s essential to distinguish pulmonary edema from pleural effusion, as both conditions involve the accumulation of fluid in the chest cavity but have different underlying causes. Pulmonary edema results from increased pressure in the blood vessels of the lungs, leading to fluid leakage into the air sacs. On the other hand, pleural effusion occurs when fluid accumulates in the space between the lungs and the chest wall. This differentiation is crucial for accurate diagnosis and appropriate treatment selection.
Pulmonary Edema Symptoms and Diagnostic Challenges
Pulmonary edema presents with a range of symptoms, including severe shortness of breath, coughing, wheezing, and a feeling of suffocation. However, these symptoms can be challenging to attribute solely to pulmonary edema, as they may overlap with other respiratory conditions. This diagnostic challenge underscores the importance of conducting a thorough physical examination, obtaining a detailed medical history, and performing diagnostic tests, such as chest X-rays and arterial blood gas analysis, to confirm the presence of pulmonary edema.
Exploring Pulmonary Edema Medications and Treatment Options
The management of pulmonary edema involves addressing both the underlying cause and the associated symptoms. Medications such as diuretics are commonly used to reduce fluid retention in the body, thereby alleviating the buildup of fluid in the lungs. In addition to diuretics, vasodilators may be prescribed to reduce the pressure in the blood vessels of the lungs. Supplemental oxygen therapy and mechanical ventilation are also vital in providing respiratory support to patients experiencing severe pulmonary edema.
Pulmonary Edema Complications and Survival Rates
Pulmonary edema can lead to life-threatening complications if left untreated. Acute respiratory distress syndrome (ARDS) and cardiogenic shock are among the severe consequences of uncontrolled pulmonary edema. The survival rates for pulmonary edema depend on various factors, including the underlying cause, the timeliness of intervention, and the overall health of the patient. Early recognition and prompt initiation of appropriate treatment significantly influence the prognosis and survival outcomes for individuals with pulmonary edema.
Uncovering Rare Types of Pulmonary Edema
While the most common form of pulmonary edema is cardiogenic, there are rare types that have distinct etiologies. Neurogenic pulmonary edema, for example, occurs as a result of severe brain injury or neurological conditions, leading to a sudden increase in pulmonary vascular permeability. Reexpansion pulmonary edema is another rare form that manifests after the rapid reexpansion of a collapsed lung, often following thoracentesis or chest tube drainage. Recognizing these rare types of pulmonary edema is crucial for tailored management and improved patient outcomes.
Special Considerations: Pulmonary Edema vs. Pneumonia
Pulmonary edema and pneumonia are both respiratory conditions that can cause significant morbidity and mortality. However, they have distinct pathophysiologies and clinical presentations. Pneumonia is characterized by lung inflammation due to infection, whereas pulmonary edema involves the accumulation of fluid as a result of heart failure or acute respiratory distress. Distinguishing between these conditions is essential for accurate diagnosis and targeted treatment strategies.
Preventing and Managing Swimming-Induced Pulmonary Edema
Swimming-induced pulmonary edema (SIPE) is a unique form of pulmonary edema that occurs during or immediately after swimming, particularly in cold water. Individuals engaged in water activities should be aware of the potential for SIPE and take preventive measures, such as acclimatization to cold water, avoiding overexertion, and recognizing early symptoms, such as coughing and breathing difficulties. If SIPE occurs, prompt removal from the water and seeking medical attention are crucial for preventing complications.
Case Studies and Insights on Negative Pressure Pulmonary Edema
Negative pressure pulmonary edema (NPPE) is a condition that develops following acute upper airway obstruction, leading to intense negative intrathoracic pressure during inspiration. Case studies and clinical insights on NPPE highlight the importance of prompt recognition and intervention to prevent severe respiratory compromise. Understanding the pathophysiology and risk factors associated with NPPE can aid healthcare professionals in implementing preventive measures and providing timely management in affected individuals.
Conclusion: Recognizing the Signs and Seeking Timely Treatment
In conclusion, the identification of pulmonary edema and its various types is essential for effective management and improved patient outcomes. Being knowledgeable about the ICD 10 code for pulmonary edema, understanding its symptoms, and differentiating it from similar conditions are critical components of accurate diagnosis and targeted treatment. By recognizing the signs early and seeking timely medical intervention, individuals at risk of pulmonary edema can receive appropriate care, potentially reducing the risk of complications and improving their overall prognosis.
If you or someone you know is experiencing symptoms of pulmonary edema, seek immediate medical attention to receive a comprehensive evaluation and appropriate treatment. Early intervention is essential for better outcomes and improved quality of life.